
What is the metabolic health crisis?
Metabolic health is getting worse for a growing number of people. Here is a look at the scale of the crisis and why we need to address it now.
What do we mean by metabolic health?
Broadly, metabolic health describes how well our body produces and uses energy. Every one of the trillions of cells in our bodies is a small powerplant that converts fuel (usually glucose or fat) to energy the body can use (typically ATP). When our cells cannot run those processes efficiently, it can lead to any number of conditions depending on what cells are suffering. In the brain, poor metabolic health can contribute to decreased mental acuity (brain fog), anxiety, or Alzheimer’s. In the blood vessels, it can contribute to microvascular disease (like erectile dysfunction and retinopathy, and kidney disease) and cardiovascular disease (like heart attacks and strokes). In the liver, non-alcoholic fatty liver disease. In many cells: cancer, which is linked to poor metabolic health. Metabolic dysfunction can even lead to obesity by interfering with our body’s fat storage and burning capabilities.
"93% of Americans are not metabolically healthy, and more than a third of US adults have prediabetes. Of those, more than 84 percent don’t know they have it."
But poor metabolic health doesn’t always manifest in overt cardiometabolic diseases. We can also feel it in pain points and symptoms of everyday life: fatigue, brain fog, depression, anxiety, lack of exercise endurance, infertility, balding, erectile dysfunction, acne, chronic pain, increased appetite, and more.
One of the most direct measures we have for metabolic health is glucose, or blood sugar, since that constitutes much of the fuel for your cells, as well as insulin, the hormone that helps our cells take in glucose. Consistently high blood sugar and impaired insulin function (called insulin resistance) are behind most of the conditions that come with poor metabolic health, including, most directly, diabetes and prediabetes.
Type 2 diabetes is advanced insulin resistance, where the body has become so insulin resistant that blood sugar climbs dangerously high, damaging parts of the body from the eyes to the muscle tissue.
So increases in diabetes and other metabolic-related chronic conditions mean that our metabolic health is getting worse. And we see a lot of increases.
10 Stats that Show Metabolic Health is Getting Worse:
1. 93% of Americans are not metabolically healthy. Using data from the National Health and Nutrition Examination Survey (NHANES) covering 1999–2018, researchers found that only 1 in 14 American adults showed optimal levels of all five metabolic risk factors: BMI, glucose, blood pressure, HDL, and triglycerides without medication. The same data showed only 37% of adults had fasting glucose under 100 mg/dL, the typical threshold for prediabetes.
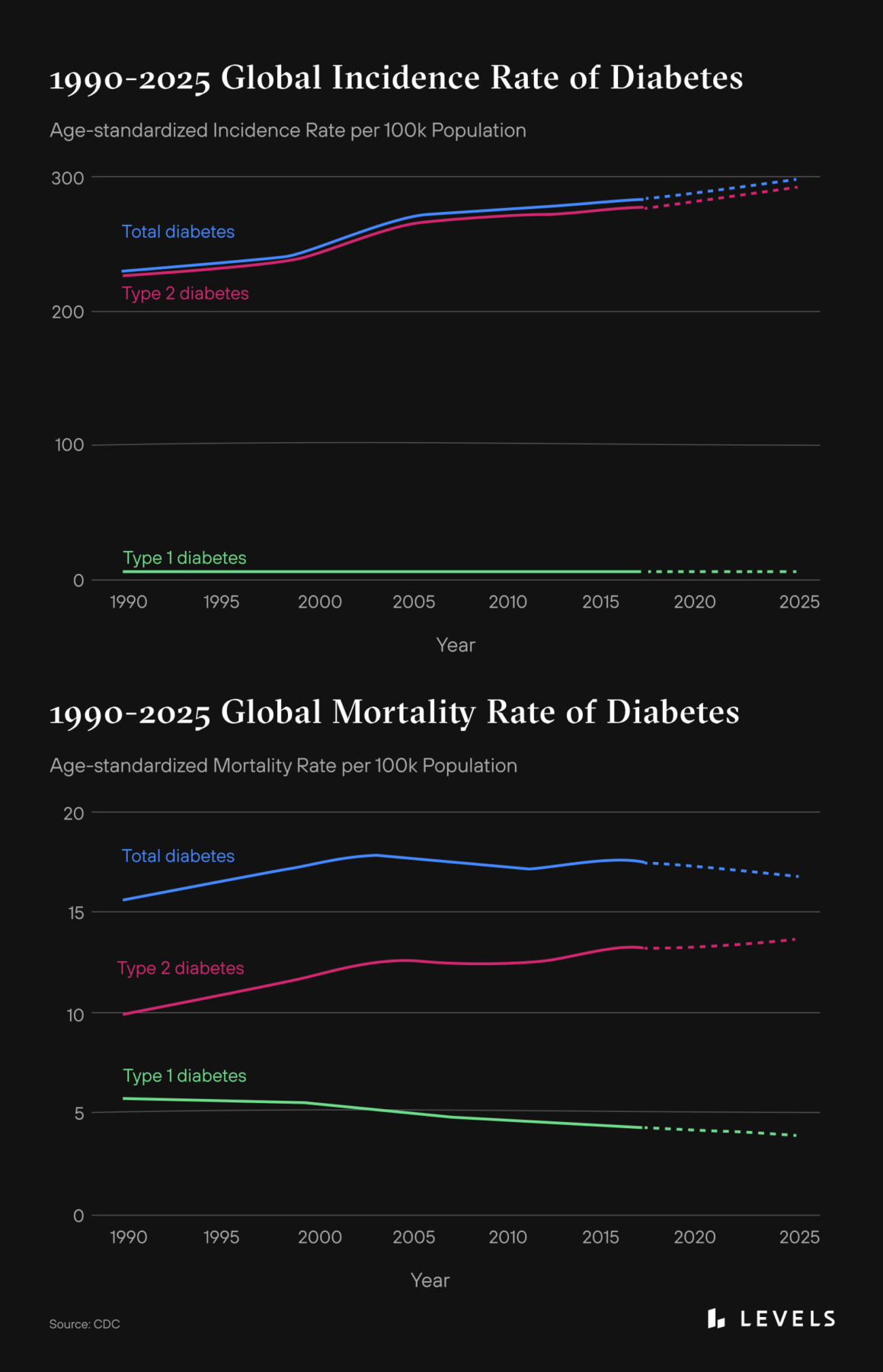
2. More than 10% of people in the US have diabetes, and 21% of that is undiagnosed**.** Worse, the incidence rate is rising globally—now at 10%—and among kids under 19, and Type 2 makes up the vast majority of those cases. The mortality rate is also increasing, even as it is decreasing for Type 1.
3. More than a third of US adults have prediabetes**.** Of those, more than 84 percent don’t know they have it. The likelihood of progression to Type 2 diabetes varies considerably depending on the person and other factors (but could be as high as 64%). However, prediabetes alone increases the risk of stroke, heart disease, and Alzheimer’s.
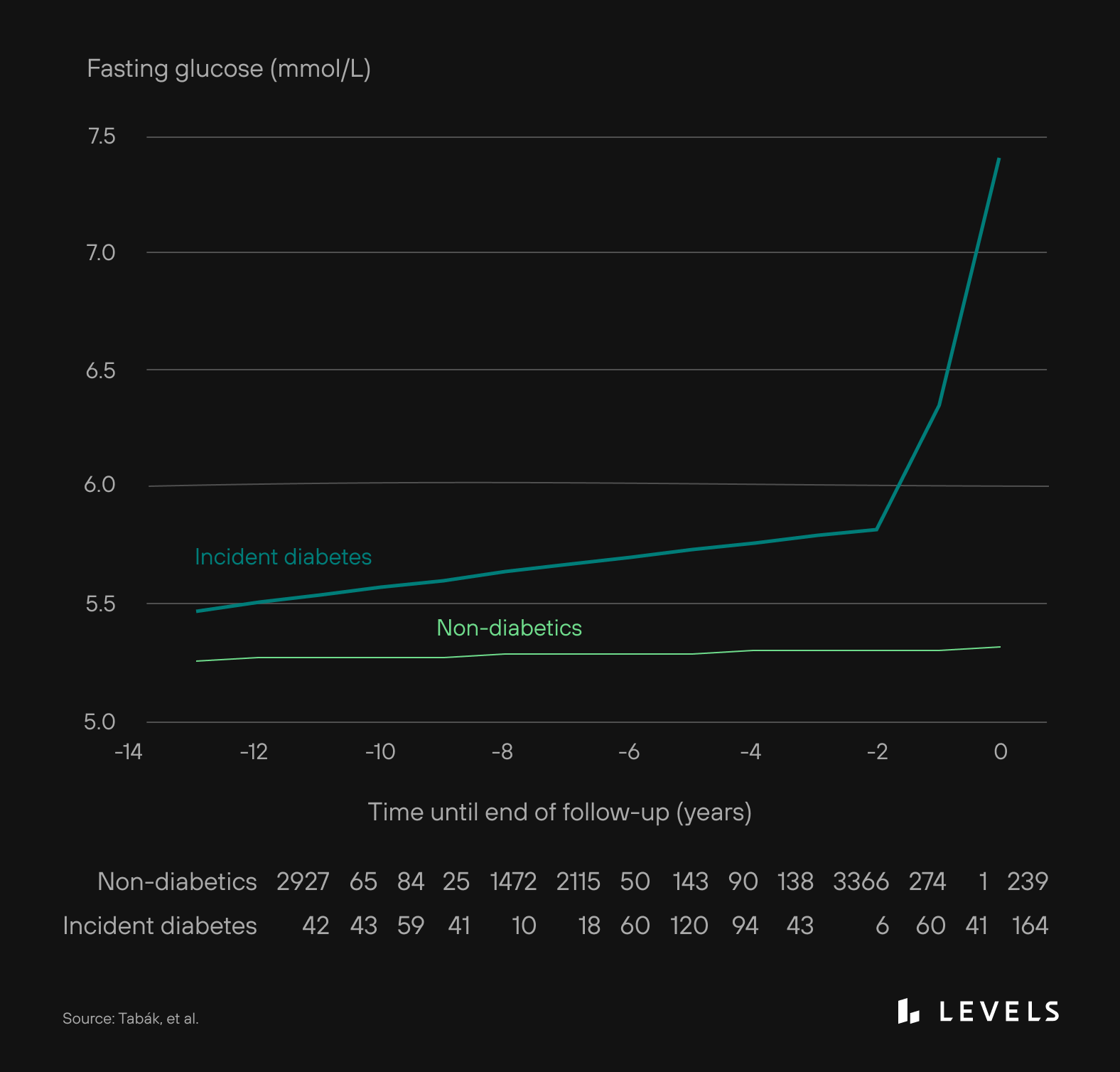
4. Insulin resistance affects more than 129 million Americans**.** This stat includes the 34.2 million people of all ages with diabetes and the 88 million who have prediabetes. It also includes another 7.3 million adults who meet laboratory criteria for diabetes but were unaware they had it. And likely, the number of people with insulin resistance in America is even higher. With early insulin resistance, your cells no longer respond well to insulin, and the pancreas produces more. But insulin resistance can begin developing up to 13 years before elevated glucose levels appear on a test.
Source: CDC
5. 73.6% of US adults are overweight or obese**.** Rates of obesity have tripled since the 1970s. While up to 30% of obese patients are metabolically healthy, abdominal obesity is associated with metabolic syndrome. Globally the prevalence of adult obesity is 13%, whereas, in the US, it’s the highest at over 35%. Researchers are still studying the underlying mechanisms. But we know that obesity is linked to insulin resistance, likely by way of lipid deposits inhibiting insulin signaling and adipose tissue producing inflammatory cytokines.
6. Around a quarter of the US suffers from preventable non-alcoholic fatty liver disease (NAFLD)**.** Globally, cases of NAFLD have more than doubled from 1990 to 2017. The US is one of five countries with the highest burden in terms of absolute case counts. Countries with a surge in obesity and diabetes over the past three decades have also seen an increase in NAFLD. Metabolic disorders are risk factors for NAFLD, which, if left untreated, can progress to end-stage liver disease.
7. High blood sugar is linked to eight of the top 10 leading causes of death in the US (pre-COVID), including cardiovascular disease, stroke, cancer, Alzheimer’s disease, chronic respiratory disease, kidney disease; there are even correlations between metabolic dysfunction and suicide. A 2017 study suggests that diabetes is the third leading cause of death rather than the seventh.
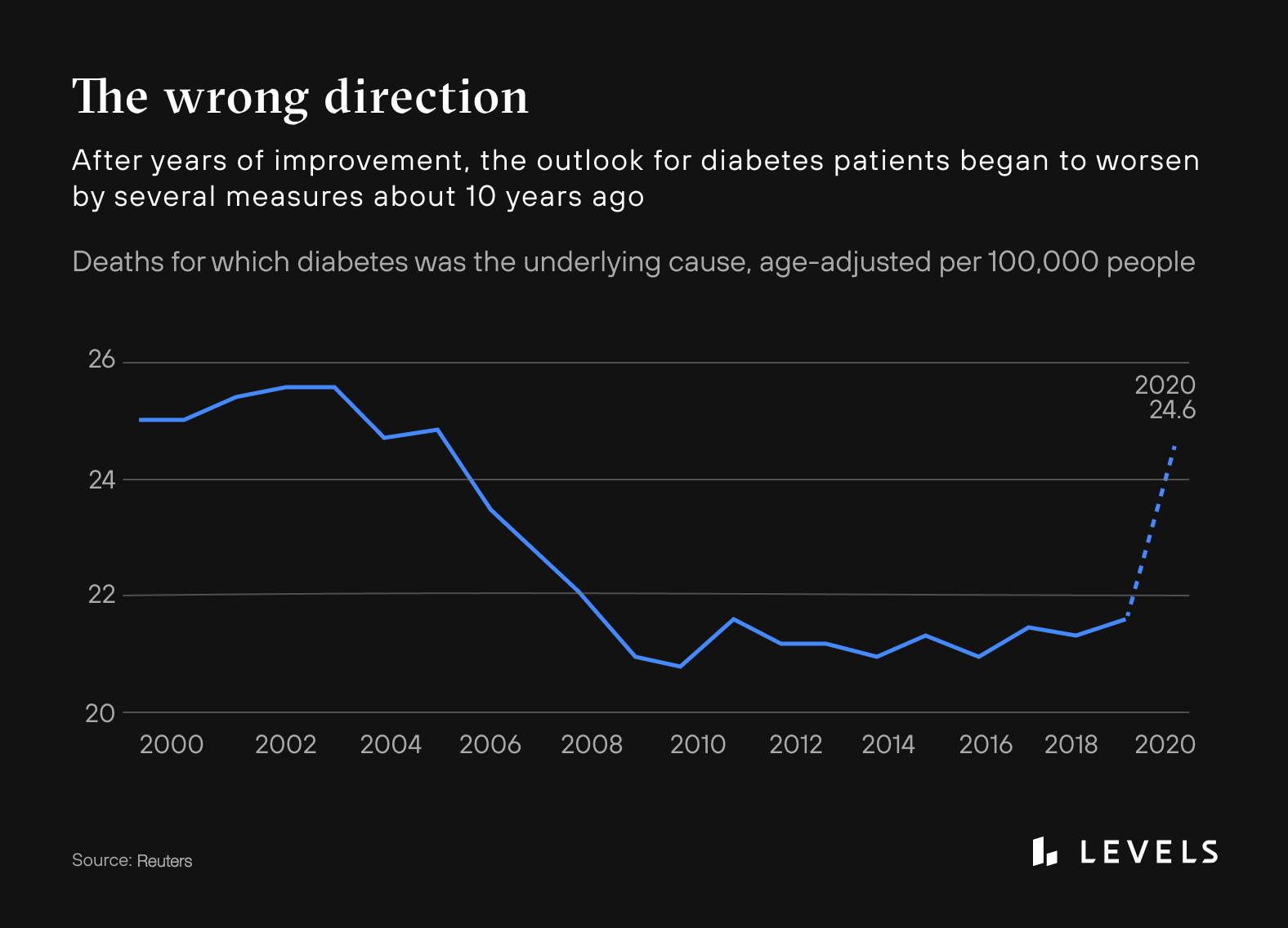
Source: Reuters
8. Individuals meeting at least three criteria for metabolic syndrome have 60% higher annual healthcare costs; diabetes alone contributes to $327 billion in medical costs and lost productivity, a number expected to exceed $600 billion by 2030. The prevalence of NAFLD in the US contributes to an estimated $100 billion in healthcare costs. If the obesity rate continues on its current trajectory, the NAFLD burden could increase to $1 trillion by the end of the decade.
9. COVID-19 became a top-three leading cause of death in 2020 and 2021, and 40% of people in the US who died from COVID had diabetes. Another study found that nondiabetic COVID-19 patients hospitalized with elevated blood sugar were three times more likely to die than those with stable glucose levels. And a new study finds that having three of more symptoms of metabolic syndrome—obesity, pre-diabetes or diabetes, hypertension and high cholesterol—when hospitalized with COVID makes you 20% more likely to die in the hospital. Researchers say the dual pandemics of metabolic syndrome and COVID-19 are linked. COVID-19 may also exacerbate the ongoing metabolic crisis or drive up Type 2 diabetes rates, as researchers have found a link between infection and persistent hyperglycemia. One study found that about 46% of patients admitted to a hospital for COVID-19 had high blood sugar during their stay. And about 35% of those patients had hyperglycemia lasting for at least six months after infection.
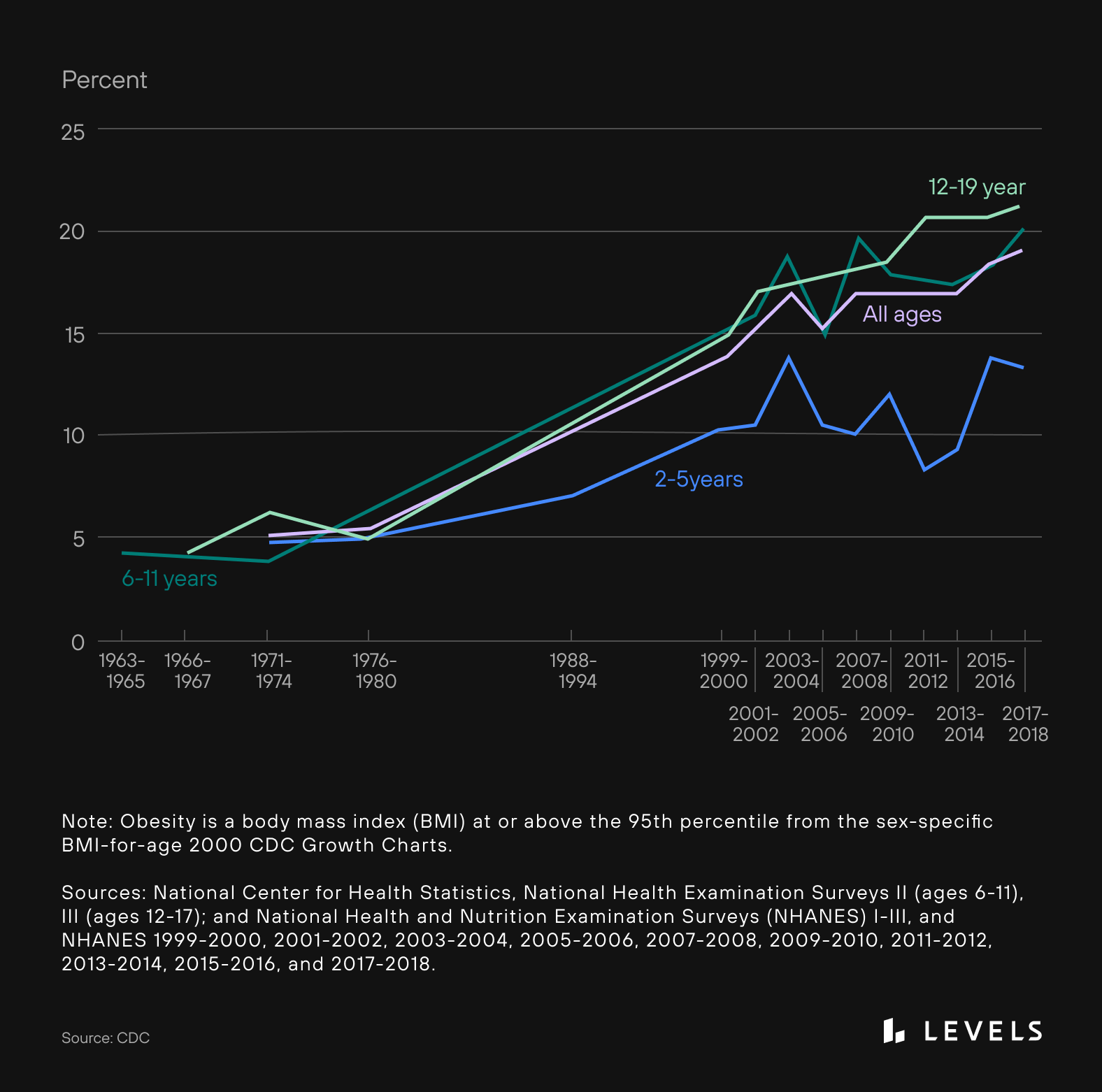
10. It’s even worse for kids. More than 20% of children age 2-19 meet the criteria for obesity**, up from 6% in the early 1970s**. The number of kids with severe obesity has grown from 1% to 6%. As many as 12% of kids globally have NAFLD, but that rate is as high as 80% among kids with obesity. Two separate research projects just found significant increases—more than doubling in one data set—in the rates of diabetes among kids during the pandemic, as well the proportion of Type 2 diabetes versus Type 1. Between 2011 and 2014, 63% of people 19 and under in the United States drank a sugar-sweetened beverage (SSB) on a given day.
Source: CDC
What’s fueling this metabolic health crisis?
How have insulin resistance, prediabetes, and Type 2 diabetes become endemic? Our genetic code has not appreciably changed in the last 100 years. Instead, our lifestyles have changed dramatically from those of even our not-so-distant ancestors—so much so that how we live now would be unrecognizable to them.
There are several contributing factors, but the inspiring (and frustrating) fact is that all of them are within our control.
- Chronic “overnutrition” broadly refers to the standard hypercaloric (and often, high-carbohydrate) diets many people now eat. Those can coexist with the double burden of malnutrition. In other words, someone can be obese or overweight but still not get proper nutrition.
- The macro- and micronutrient needs of the human body haven’t changed dramatically in the last several hundred years. Yet, we have an ever-increasing amount of food choices available to us, whether at a grocery store, a restaurant, or a drive-through. Our bodies haven’t adapted to cope with this level of incoming energy—especially from processed foods.
- We eat nearly 10x more sugar per day than we did 100 years ago. Sugar stimulates the pancreas to make insulin (the hormone that aids cells in glucose uptake). But cells can eventually become unresponsive to insulin. Insulin resistance is at the core of many chronic diseases, and it leads to excess glucose being converted to fat and stored in the liver, contributing to NAFLD.
- We are more sedentary than ever. Research shows that from 2001 to 2016, Americans increased their total sitting time. And from 2010 to 2015, only about 23% of adults 18 to 64 met the federal guidelines for aerobic and strengthening activities. The COVID-19 pandemic, which has required widespread remote learning and working from home, has exacerbated the trend of increased sitting and decreased physical activity, especially for children.
- We seem to get less sleep, which has consequences for our metabolic health. The prevalence of shorter sleep times, characterized by getting less than seven hours, increased from 2013 to 2017. Inadequate sleep is linked to obesity, Type 2 diabetes, heart disease, and even death.
- We’re increasingly exposed to environmental pollution and metabolism-disrupting chemicals. After years of somewhat declining levels of fine particulate pollution, we saw a worsening of America’s air quality with an increase in a type called PM2.5 in 2020. PM exposure is associated with systemic inflammation that may result in metabolic syndrome or exacerbate existing dysfunction. And our exposure to bisphenol A (BPA), phthalates, perfluoroalkyl substances (PFAS), pesticides, antifouling agents, and more has consequences for our mitochondria.
- Ultra-processed foods make up 60% of the calories Americans eat. Yet high consumption of ultra-processed foods increases one’s risk of becoming overweight or obese by up to 39% and developing metabolic syndrome by up to 79%. In 2016, adults consumed more than 14% of their calories from added sugar. When the body gets too much fructose, as is present in high fructose corn syrup, the liver can start turning the excess sugar into fat, contributing to NAFLD.
- The experience of psychological stress appears to be increasing. Stress kicks off a hormonal cascade that promotes fat storage and impairs glucose control. Chronic psychological stress and higher levels of the stress hormone cortisol are also linked to insulin resistance. Cortisol signals the liver to release stored glucose, but it also makes it harder for insulin to signal cells for glucose uptake, creating a problematic cycle.
- Late night eating can result in insulin resistance. Post-meal glucose levels and insulin are elevated at night when compared to meals consumed earlier in the day. And without physical activity before bed, the body takes longer to clear a glucose load. Snacking can lead to frequent blood sugar spikes. But eating fewer meals may improve insulin sensitivity.
What Can We Do About It?
As individuals:
- Eat a metabolically healthy diet. Eating in a way that regulates your blood glucose levels rather than causing spikes and dips can help mitigate or reverse insulin resistance. And it can even help control cravings and boost weight loss if that’s your goal. Focus on whole foods (not processed). Avoid added sugar, and eat low glycemic index foods. Pair carbohydrates with fat, fiber, or protein. This method can head off a blood sugar spike and slow energy absorption, staving off hunger.
- Get exercise. Movement matters, so find something you love to do and keep doing it regularly. While the CDC recommends at least 150 minutes of moderate exercise per week, more is great. Low-intensity movement is powerful enough to help improve the way the body processes glucose. And a post-meal walk can help mitigate a spike.
- Reduce stress. Our stress hormones (cortisol, adrenaline, and epinephrine) signal the liver to create or release glucose to fuel our body so we can respond in fight-or-flight mode. But nowadays, we’re unlikely to be running from a predatory animal. Instead, our triggers are often professional or social, leading to an elevated blood sugar level while we sit and stress. Repeated stress makes the liver more insulin resistant. Research shows that mindfulness practices, like twice-weekly meditations or 20-minute daily breathing, can reduce glucose levels and improve glucose processing. Plus, these habits can help your body better cope when worry or tension arise.
- Get healthy sleep. Aim for eight hours of sleep each night, seven at the minimum. Less than six hours of sleep is associated with metabolic syndrome and higher waist circumference.
As a society:
- Better Dietary Guidelines for Americans. We need DGAs that are updated more regularly and follow the latest nutrition and health science rather than cater to American agriculture.
- Better “safety-net” food programs. The DGA helps inform which foods are available for Child and Adult Care Food Programs (CACFP), Supplemental Nutrition Assistance Program (SNAP), and Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). SNAP, for example, has historically featured a narrow range of foods, limiting nutritional options. A 2017 study published in the American Journal of Public Health found that SNAP participants have higher total and cardiovascular disease mortality when compared to people who are ineligible for the program or eligible but don’t participate.
- Better school lunches. On average, 11% of calories from school lunches are from added sugar, according to a new study published in Nutrients. The top source is flavored milk, accounting for nearly half of added sugars. Other sources include condiments and toppings, as well as breads, rolls, and bagels. Tomato paste/sauce, which has added sugar, is considered a vegetable. The United States Department of Agriculture (USDA) and the Department of Health and Human Services (HHS), which release the DGA every five years, ignored the advice of the DGA advisory committee to make the recommendation for added sugar to less than 6% of calories for anyone ages one and up. Instead, the 2020–2025 DGA lists the added sugar limit as 10%.
- Fewer subsidies for unhealthy foods. The seven major subsidized foods in American Agriculture are corn, soybeans, wheat, rice, sorghum, dairy, and livestock. A recent study published in JAMA Internal Medicine looked at National Health and Nutrition Examination Survey data from 2001 to 2006 of more than 10,000 adults. The study found that adults who ate higher food commodities had a higher probability of cardiometabolic risks.
- Increase nutrition education in medical school. Even though dietary habits are a key contributor to health outcomes, nutrition education is lacking in medical training around the globe, according to research published in The Lancet Planetary Health.

Take control of your metabolic health
Levels helps you see how food and lifestyle affect your health through macro tracking, habit-building, and customized insights and advice. Levels members can also incorporate biomarker data like real-time glucose and metabolic blood testing for an even more personalized experience. Click here to get started with Levels.





