
New study asks whether umami flavor causes metabolic dysfunction
Researchers uncover the molecular connection between MSG and obesity in mice, but whether the findings extend to humans is still unclear.
Video breakdown: 5 Minutes, 5 Slides, 5 Questions
The Study:
“Umami-induced obesity and metabolic syndrome is mediated by nucleotide degradation and uric acid generation”
Published: Nature Metabolism, September 2021
Where: University of Colorado School of Medicine
The Takeaway:
Umami flavor, at least when delivered via MSG, may negatively affect metabolic health in mice.
There are five different human tastes; sweet, salty, savory (umami), bitter, and sour. If given the opportunity, humans tend to avoid the bitter and sour and select sweet, salty, or savory-tasting food. While we know that excessive consumption of sweet and salty flavored foods leads to metabolic and cardiovascular dysfunctions, we don’t know whether umami-tasting foods have a similar negative consequence. In this study, the researchers found that in mice, adding monosodium glutamate (MSG) in their drinking water was sufficient to increase caloric intake and metabolic syndrome, similar to the effects of fructose. The molecular mechanism responsible for the metabolic consequences is tissue-specific (brain or liver) activation of an enzyme important in the breakdown of glutamate (a part of MSG) called AMPD2.
"The researchers suggest that overconsumption of umami flavor might have detrimental effects in modern society, similar to how overconsumption of fructose and sweet flavor leads to chronic overnutrition or how increased salt consumption leads to hypertension and metabolic dysfunction."
Overall, the authors appear to demonstrate that umami taste—mediated by glutamate—is detrimental to the metabolic health of mice. Future studies will show whether cutting umami-flavored food improves metabolic health in humans as well.
What It Looked At:
Umami is a savory, rich flavor that only joined the sour, bitter, sweet, and salty flavors in 2002 when umami-specific taste receptors were found on the human tongue. The specific molecule that activates the savory umami flavor is glutamate. Some savory flavored foods with glutamate include mushrooms, tomatoes, onion, sweet peas, and meats such as sardines, beef, and chicken. Not exactly foods associated with poor health typically.
However, the researchers cite previous research in the introduction that infants will preferentially choose umami, sweet, and salty flavors over bitter and sour flavors. This suggests that perhaps umami flavor promotes the consumption of specific foods critical for our ancestors’ survival, similar to sweet and salty foods. The researchers suggest that overconsumption of umami flavor might have detrimental effects in modern society, similar to how overconsumption of fructose and sweet flavor leads to chronic overnutrition or how increased salt consumption leads to hypertension and metabolic dysfunction.
Umami flavor is mediated by a metabolite called glutamate that binds the glutamate taste receptors. The amount of free glutamate in food can be modified during the ripening, drying, curing, and cooking stages and is a component of MSG, a common food seasoning. Interestingly, glutamate more strongly binds the glutamate receptor in the presence of the purine metabolites IMP, AMP, and GMP. Purine metabolism is involved in the production of uric acid and, over time, can lower ATP levels in the cell, which are linked to metabolic syndrome and cardiovascular disease. Thus, several potential mechanisms might link umami-flavored foods to metabolic dysfunction.
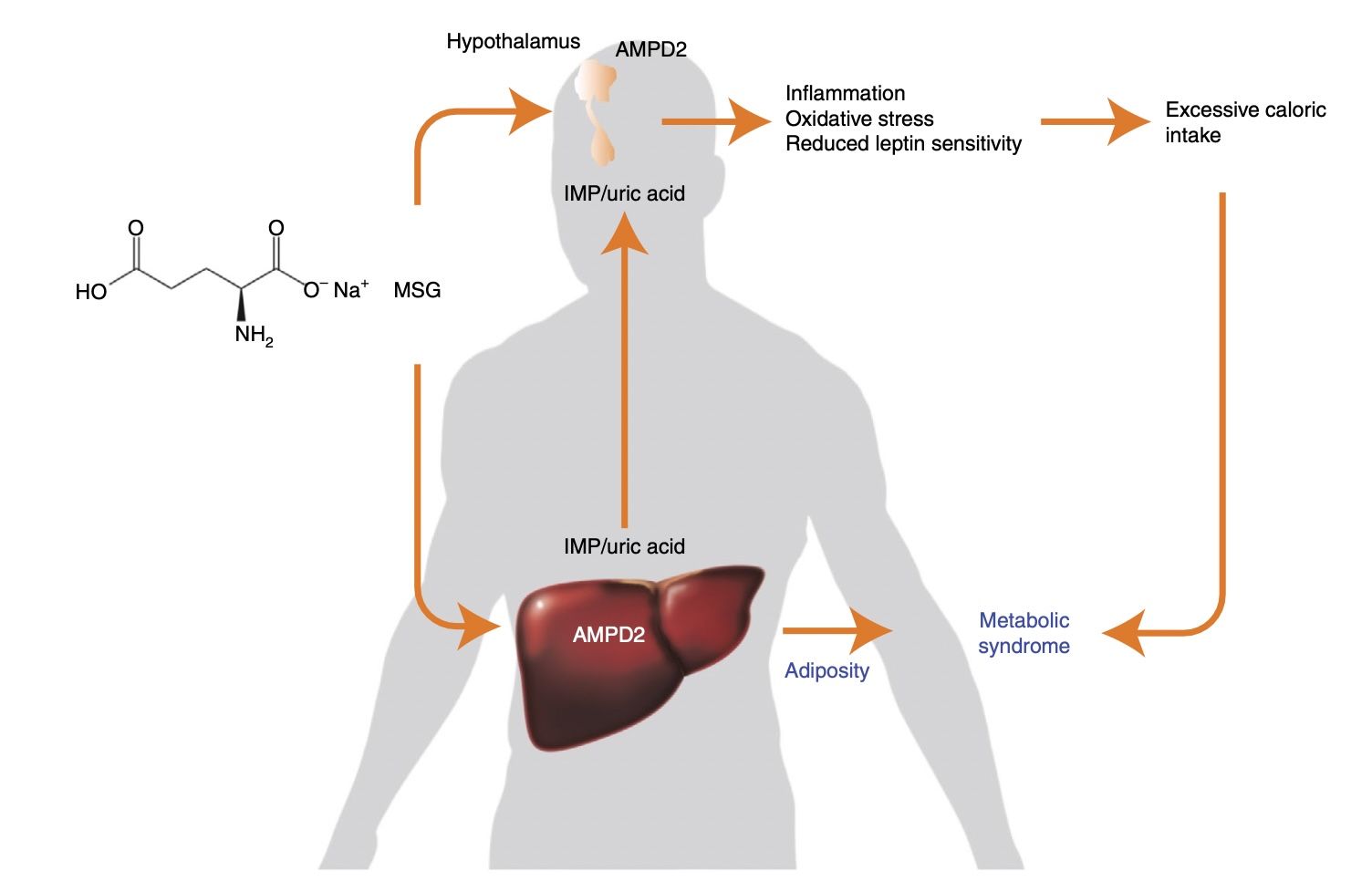
Proposed mechanism for MSG-induced metabolic syndrome. The addition of purines to MSG markedly exacerbates the intake of glutamate. excessive glutamate is metabolized in the liver and hypothalamus to glutamine and ultimately IMP via the purine pathway with consumption of ATP and formation of AMP. IMP formed from both glutamine and AMP via AMPD2 enters the purine degradation pathway to generate uric acid and consequently oxidative stress and inflammation. Activation of AMPD2 in the liver drives metabolic dysfunction and adiposity while providing uric acid and IMP. Activation of AMPD2 in neurons induces inflammation and oxidative stress and reduces the sensitivity of hypothalamic neurons to leptin causing hyperphagia. Increased caloric intake and the promotion of metabolic dysfunction are the underlying factors whereby MSG and purines may cause metabolic syndrome. Image and caption source: Andres-Hernando, et. al.
The researchers conducted all of their experiments in mice and utilized several genetic and pharmacological interventions to find how glutamate caused the metabolic syndrome. Here is a (partial) list of approaches that they took along with the scientific rationale:
- Feeding normal mice increased concentrations of MSG. This was a proof of concept that MSG could induce weight gain.
- Feeding MSG to mice that lacked an important purine enzyme, AMPD2, in the hypothalamic region of the brain. This tested whether MSG increased appetite via the brain.
- Feeding MSG to mice that lacked AMPD2 only in the liver. This tested whether MSG increased metabolic dysfunction via the liver, which plays a crucial role in metabolism in mice (and, to a lesser degree, in humans).
- Feeding MSG to mice that had AMPD2 during development but then lost functional AMPD2 after they had already developed MSG-mediated metabolic dysfunction. This tested whether MSG-induced metabolic dysfunction could be reversed (rather than just prevented) if AMPD2 were eliminated.
- Feeding MSG and IMP to mice without AMPD2 and mice with intact AMPD2. This tested whether other purines were also dependent upon AMPD2 activity for their adverse effects.
In addition, the researchers measured many metabolites and performed many experiments for each of these mouse experiments, including:
- Body weight, fat mass, fat weight, liver weight.
- Food intake, water intake, preferences for MSG-flavored water.
- Metabolites such as insulin, leptin, triglycerides, uric acid, ATP.
- Oral glucose tolerance test and insulin tolerance test to measure metabolic function.
- Enzymes such as AMPD2, AST (a marker of liver damage).
As you can see, this was an extensive study with several measurements and mechanisms examined. Let’s take a look at the results.
What It Found:
Increased MSG can drive obesity. In the first mouse study, researchers provided the mice with increasing amounts of MSG in their drinking water and found that more MSG led to more food intake, increasing body weight and uric acid in the liver. The increased intake of glutamate (from MSG) increased a particular pathway, called the purine biosynthesis pathway, which results in lower ATP levels and terminates in increased uric acid. A key enzyme in purine biosynthesis is the AMPD2 enzyme.
Both the liver and brain seem to play a role in MSG’s metabolic effects. In the next set of experiments, the researchers genetically blocked the AMPD2 enzyme in all tissues in the mice. When these mice consumed MSG, they did not increase food intake, and their uric acid levels were lower than in mice with functional AMPD2.
Next, researchers tried to tease out which specific tissues (brain, muscle, liver) were responsible for these effects. When they blocked AMPD2 activity only in the brain, the MSG-fed mice didn’t eat more, preferred the MSG water over plain water, or had an increase in uric acid.
Then the researchers turned to the liver. In a control group of mice, they had found that MSG increased liver fat content. But when the researchers genetically blocked the AMPD2 activity in the liver, they saw many of the same effects as the other experiments: lower food intake, less weight gain, less fat mass, and less damaged livers.
Their interpretation: AMPD2 inactivation in the brain or liver has similar overall effects of preventing the MSG-mediated metabolic syndromes but did so via different molecular mechanisms: Reduced appetite in the brain and reduced metabolic stress in the liver.
MSG-induced metabolic dysfunction can be reversed. In previous genetic models, the researchers eliminated AMPD2 for the mice’s entire lives and thus prevented MSG-mediated metabolic dysfunction. Here they wanted to show that reducing AMPD2 activity could also reverse the effects of MSG. To do so, they used a common genetic trick in which they fed the mice a specific drug that would “turn off” AMPD2 enzyme activity. Researchers added MSG to the mice’s water for 7 weeks to induce metabolic dysfunction, and only then did they “shut off” AMPD2. That led the mice to cut caloric intake, stop gaining fat and overall weight, and it reduced blood levels of triglycerides, insulin, and leptin (a satiety hormone produced by adipose tissue).
Umami flavors play a role in appetite. When researchers added IMP, a purine that can enhance the umami flavor from glutamate, to a low level of MSG in the mices’ water, they found the mice had an increased preference for MSG, increased food intake, impaired glycemic control, and lower insulin sensitivity compared to mice who got only MSG with no IMP.
The critical mechanism appears to be leptin, a hormone that suppresses appetite. The IMP-fed mice showed inflammation in the brain, which is thought to be associated with leptin resistance (Incidentally, these effects could be reversed when they blocked AMPD2 in the brain, suggesting a role for AMPD2 in mediating some of the effects of leptin.) These results suggested an essential role for umami flavors to regulate appetite.
Uric acid plays a role in the harmful effects of MSG. In other tests, uric acid plus MSG resulted in more severe metabolic consequences, but when researchers blocked uric acid formation, they could reverse many of the detrimental effects of MSG plus uric acid, as well as those caused by MSG plus IMP. Uric acid is thought to induce metabolic dysfunction by generating oxidative stress in the mitochondria that impairs fatty acid oxidation and stimulates lipogenesis (fat creation).
Why It Matters:
While we know some aspects of how nutrition and physical inactivity drive the metabolic health crisis, we know there are likely other contributing mechanisms. This study suggests that too many umami-flavored foods may be one such contributor.
Remaining Questions:
The entirety of these data was collected in mice. While the researchers offer biologically feasible mechanisms for the results, the limited data in humans is more nuanced and inconclusive than “umami is bad for us.”
- A 2014 paper showed that umami flavor increased appetite (similar to the mice) immediately after consuming it, but that MSG also increased satiety when the meal was complete, which might lower later caloric consumption.
- Another study in 2018 showed that consumption of an umami-flavored vegetable broth supplemented with MSG for four weeks diminished the desire for umami and savory-flavored foods, which is opposite of what was found in this study in mice.
- A review paper in 2020 attempted to summarize the potential effects, both pro and con, of umami. The authors cited 13 different positive and negative impacts ranging from improving gut health to inducing liver toxicity, with no overwhelming winner in the pro/con debate.
The biology in humans is complex. Much more work needs to be done before we can confidently add umami to the sweet and salty-tasting foods tightly associated with metabolic disease.
Conclusion:
The linking of umami flavoring to metabolic diseases via existing known molecular mechanisms is a very novel finding. The researchers used an impressive number of approaches to uncover a plausible and thought-provoking molecular mechanism that could play a role in the metabolic health crisis.
Still, given how difficult it is to translate findings in mouse models to human diseases, there is no reason to panic if you are a fan of MSG, earthy mushrooms, or aged cheeses. Existing human data around umami flavor and metabolic disease are inconclusive, and it will take several better-designed studies before we can confidently advise against consuming umami flavors.
For now, we should continue to avoid what we know we should avoid—added sugars and processed foods—while satisfying that savory craving with whole foods, micronutrient-dense foods like roasted mushrooms, and broccoli.

Take control of your metabolic health
Levels helps you see how food and lifestyle affect your health through macro tracking, habit-building, and customized insights and advice. Levels members can also incorporate biomarker data like real-time glucose and metabolic blood testing for an even more personalized experience. Click here to get started with Levels.




