
Taking steroids? Expect glucose turbulence
A discussion of the different ways that steroid medications can cause high glucose levels and erratic readings on your continuous glucose monitor (CGM).
We’ve had a number of customers who have had to take short courses of steroids for various medical conditions, and have seen huge swings in their glucose levels. It can be somewhat frightening and disheartening if you aren’t expecting it. This article will dive into why this happens.
> “Oral and intravenous are the most likely to have a significant effect on glucose levels and metabolism.”
How do oral steroids affect my glucose levels?
Individuals who find themselves taking oral steroids like predisone for a medical condition are likely to see their blood sugar go haywire while on the medication. There are many different ways of getting steroids in the body, like oral (pills), inhaled, liquid drops (eyedrops), topical (creams and lotions), and intravenous. Depending on the condition, a particular route may be favored over another. For a poison ivy rash, a cream might be ideal. For severe asthma, inhaled or intravenous might. For chronic sinusitis, oral pills may be prescribed. For styes, a eyedropper liquid form might be used. Oral and intravenous are the mostly likely to have a significant effect on glucose levels and metabolism.
Steroids are generally prescribed for their anti-inflammatory and immune suppressing properties, but have several side effects, of which one of the most severe is hyperglycemia (high blood glucose).
One of our founders who normally has extremely stable glucose levels had to take a week of prednisone for a respiratory illness. His normal flat line glucose went from this:
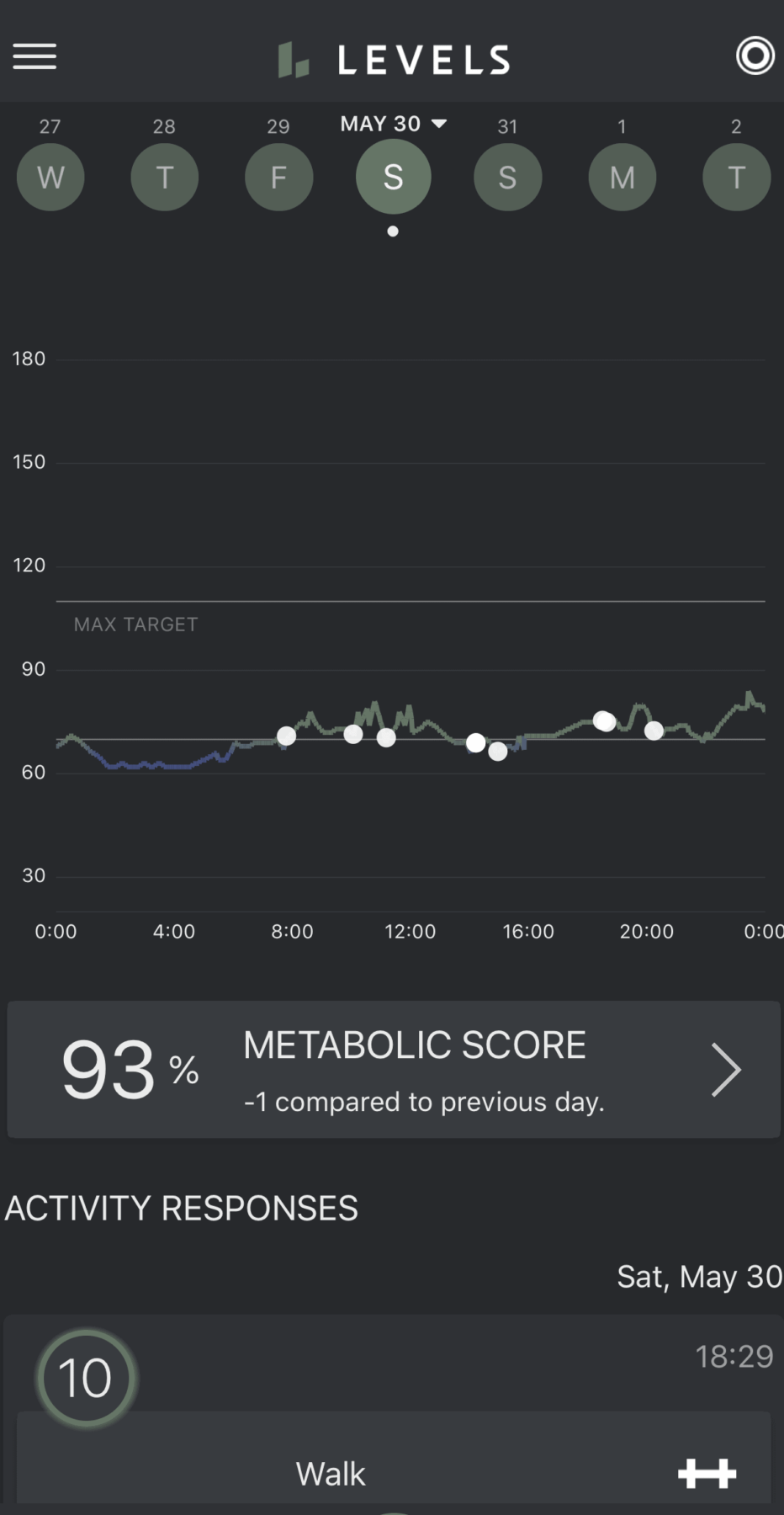
Stable, low glucose levels in the 60-70 mg/dL range
…to this:
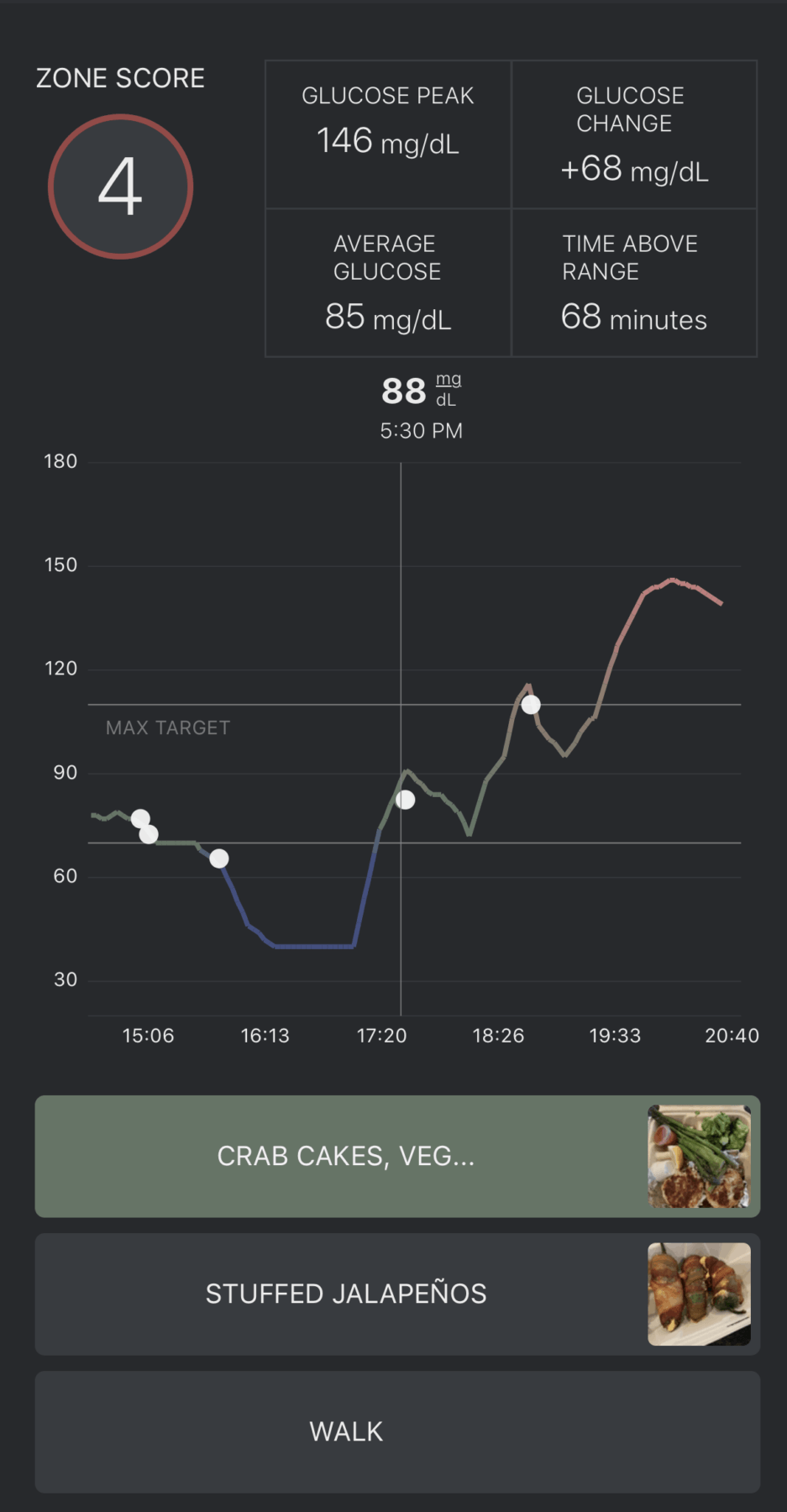
Highly erratic glucose with large swings up to 150 mg/dL
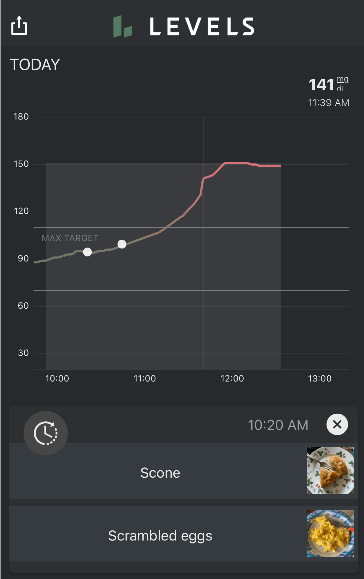
Exaggerated elevation of glucose with slow return to normal
Oral steroids affect glucose regulation through a number of different mechanisms, all of which can lead to increased glucose levels in the blood. Here are some of the main causes:
- Steroids induce insulin resistance by directly interfering how the cells absorb glucose. Specifically, steroids inhibit signaling of the GLUT4 glucose transporter channel within muscle cells, resulting in 30%-50% reduction in insulin-stimulated glucose uptake in the cells, and a 70% reduction in insulin-stimulated glycogen synthesis (glucose storage). Both of these lead to more glucose floating around in the blood stream, and less ability of the cells to take up glucose after eating.
- Steroids are responsible for the breakdown of proteins in the body, with the resulting increase in serum amino acids (amino acids are the building blocks of proteins). High levels of serum amino acids also interfere with insulin signaling in the muscle cell, leading to less glucose uptake, and more floating in the blood.
- Finally, steroids increase fat breakdown (lipolysis), resulting in an increase in blood levels of free fatty acids and triglycerides. The elevation of free fatty acids and triglycerides promote the accumulation of fats inside the cells (specifically in the form of acetyl coenzyme A, diacylglycerol and ceramide), which causes reduction of the ability of the cell to take up and store glucose.
- Steroids reduce insulin synthesis in the pancreatic beta-cells and it is thought that they reduce pancreatic cell size through the induction of beta cell death.
- Additional mechanisms, detailed in this paper.
With all of these impairments in normal glucose uptake and management, the result can be very erratic readings on continuous glucose monitors. While steroids can be lifesaving, it is important to be on minimal effective dose for as few days as possible to minimize these side effects.
Check out the following video that one of our early customers Ali Spagnola made about her experience taking oral steroids for a rash while wearing Levels:




